This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I'm Dr F. Perry Wilson of the Yale School of Medicine.
Let's be honest: Although as physicians we have the power of the prescription pad, so much of health, in the end, comes down to lifestyle. Of course, taking a pill is often way easier than changing your longstanding habits. And what's worse, doesn't it always seem like the lifestyle stuff that is good for your health is unpleasant?
Two recent lifestyle interventions that I have tried and find really not enjoyable are time-restricted eating (also known as intermittent fasting) and high-intensity interval training, or HIIT. The former leaves me hangry for half the day; the latter is, well, it's just really hard compared with my usual jog.
But given the rule of unpleasant lifestyle changes, I knew as soon as I saw this week's study what the result would be. What if we combined time-restricted eating with high-intensity interval training?
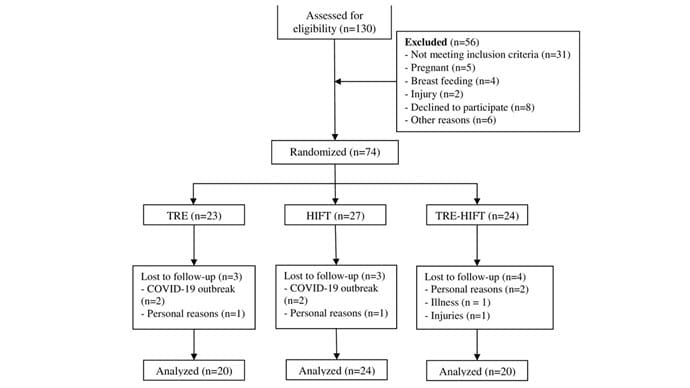
I'm referring to this study, appearing in PLOS ONE from Ranya Ameur and colleagues, which is a small trial that enrolled otherwise healthy women with a BMI > 30 and randomized them to one of three conditions.
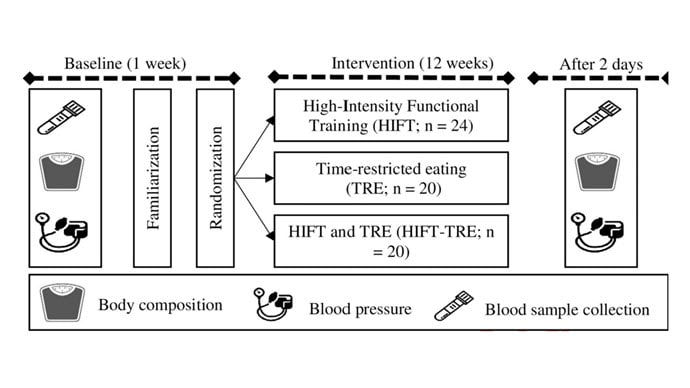
First was time-restricted eating. Women in this group could eat whatever they wanted, but only from 8 AM to 4 PM daily.
Second: high-intensity functional training. This is a variant of high-intensity interval training which focuses a bit more on resistance exercise than on pure cardiovascular stuff but has the same vibe of doing brief bursts of intensive activity followed by a cool-down period.
Third: a combination of the two. Sounds rough to me.
The study was otherwise straightforward. At baseline, researchers collected data on body composition and dietary intake, and measured blood pressure, glucose, insulin, and lipid biomarkers. A 12-week intervention period followed, after which all of this stuff was measured again.
Now, you may have noticed that there is no control group in this study. We'll come back to that — a few times.
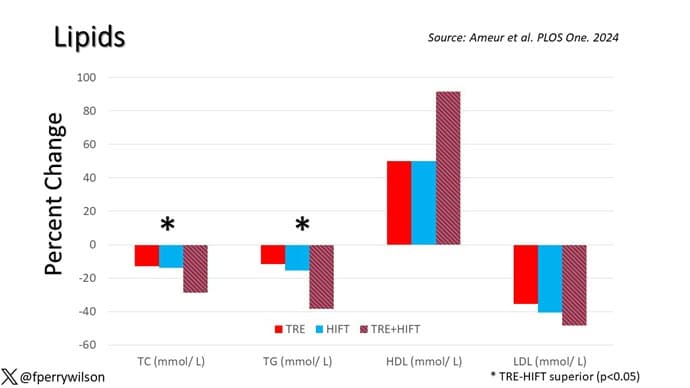
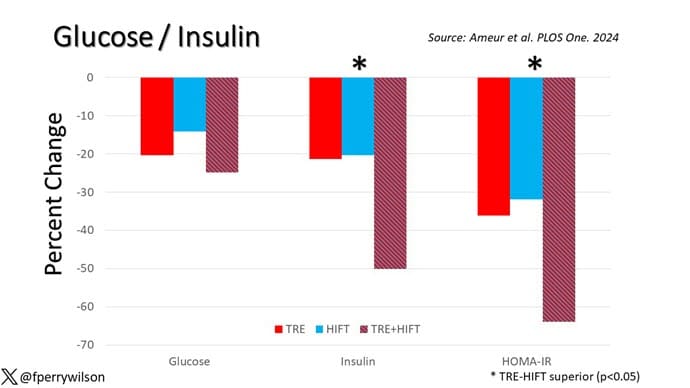
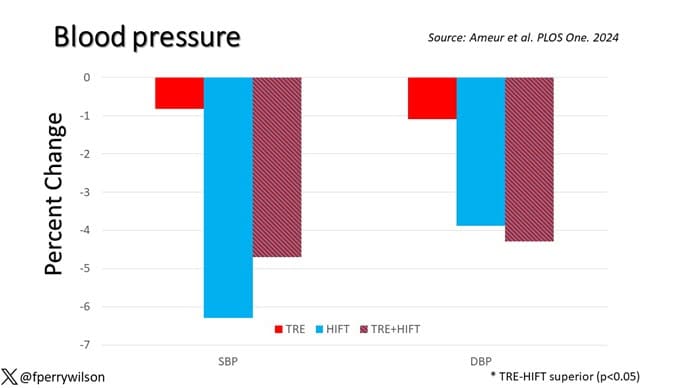
I have translated the numbers in the paper to percent changes to make things graphable and a little bit more interpretable. Let me walk you through some of the outcomes here.
First off, body composition metrics. You can see that all three groups lost weight — on average, around 10% of body weight which, for a 12-week intervention, is fairly impressive. BMI and waist circumference went down as well, and, interestingly, much of the weight loss here was in fat mass, not fat-free mass.
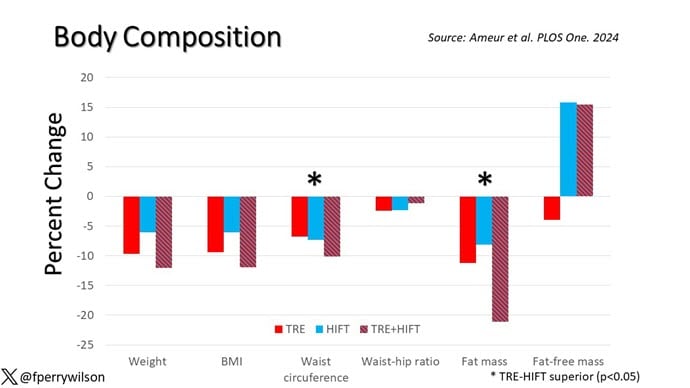
Most interventions that lead to weight loss — and I'm including some of the newer drugs here — lead to both fat and muscle loss. That might not be as bad as it sounds; the truth is that muscle mass increases as fat increases because of the simple fact that if you're carrying more weight when you walk around, your leg muscles get bigger. But to preserve muscle mass in the face of fat loss is sort of a Goldilocks finding, and, based on these results, there's a suggestion that the high-intensity functional training helps to do just that.
The dietary intake findings were really surprising to me. Across the board, caloric intake decreased. It's no surprise that time-restricted eating reduces calorie intake. That has been shown many times before and is probably the main reason it induces weight loss — less time to eat means you eat less.
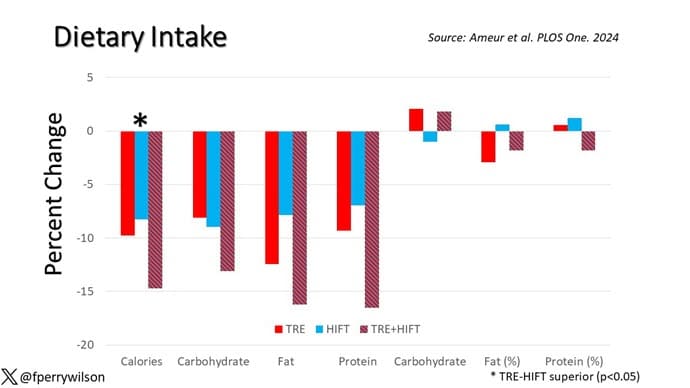
But why would high-intensity functional training lead to lower caloric intake? Most people, myself included, get hungry after they exercise. In fact, one of the reasons it's hard to lose weight with exercise alone is that we end up eating more calories to make up for what we lost during the exercise. This calorie reduction could be a unique effect of this type of exercise, but honestly this could also be something called the Hawthorne effect. Women in the study kept a food diary to track their intake, and the act of doing that might actually make you eat less. It makes it a little more annoying to snack a bit if you know you have to write it down. This is a situation where I would kill for a control group.
The lipid findings are also pretty striking, with around a 40% reduction in LDL across the board, and evidence of synergistic effects of combined TRE and high-intensity training on total cholesterol and triglycerides. This is like a statin level of effect — pretty impressive. Again, my heart pines for a control group, though.
Same story with glucose and insulin measures: an impressive reduction in fasting glucose and good evidence that the combination of time-restricted eating and high-intensity functional training reduces insulin levels and HOMA-IR as well.
Really the only thing that wasn't very impressive was the change in blood pressure, with only modest decreases across the board.
Okay, so let's take a breath after this high-intensity cerebral workout and put this all together. This was a small study, lacking a control group, but with large effect sizes in very relevant clinical areas. It confirms what we know about time-restricted eating — that it makes you eat less calories — and introduces the potential that vigorous exercise can not only magnify the benefits of time-restricted eating but maybe even mitigate some of the risks, like the risk for muscle loss. And of course, it comports with my central hypothesis, which is that the more unpleasant a lifestyle intervention is, the better it is for you. No pain, no gain, right?
Of course, I am being overly dogmatic. There are plenty of caveats. Wrestling bears is quite unpleasant and almost certainly bad for you. And there are even some pleasant things that are pretty good for you — like coffee and sex. And there are even people who find time-restricted eating and high-intensity training pleasurable. They are called masochists.
I'm joking. The truth is that any lifestyle change is hard, but with persistence the changes become habits and, eventually, those habits do become pleasurable. Or, at least, much less painful. The trick is getting over the hump of change. If only there were a pill for that.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale's Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his book, How Medicine Works and When It Doesn't, is available now.
Credits:
Image 1: PLOS
Image 2: Ameur et al., PLOS ONE
Image 3: Ameur et al., PLOS ONE
Image 4: F. Perry Wilson, MD, MSCE
Image 5: F. Perry Wilson, MD, MSCE
Image 6: F. Perry Wilson, MD, MSCE
Image 7: F. Perry Wilson, MD, MSCE
Image 8: F. Perry Wilson, MD, MSCE
Image 9: Vivian Killilea/Getty Images for Homeboy Industries
Image 10: Alamy
Medscape © 2024 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Intermittent Fasting + HIIT: Fitness Fad or Fix? - Medscape - May 01, 2024.











Comments