Abstract and Introduction
Abstract
Concerns regarding the perioperative management of acute psychostimulant intoxication have been recognized for decades, but novel and diverse substances in this class continue to be developed. Despite the similarities in mechanisms of action among psychostimulants, each subclass within this broad category has unique receptor specificity and different mechanisms that play a role in patient clinical presentation. These issues present challenges to anesthesia providers when caring for patients with either acute or chronic exposure to psychostimulants during the perioperative period. Challenges result from both physiological and psychological effects that influence the action of the primary anesthetic agent, adjuvant anesthetics, and analgesics used for perioperative management of pain. The epidemiology, pharmacology, and perioperative implications of psychostimulant use are presented for amphetamines and similar acting nonamphetamines, cocaine, and, finally, the mixed-action drugs known as entactogens that share stimulant and psychedelic properties. This information is then used as the foundation for safe and effective perioperative management of patients exposed to psychostimulants.
Introduction
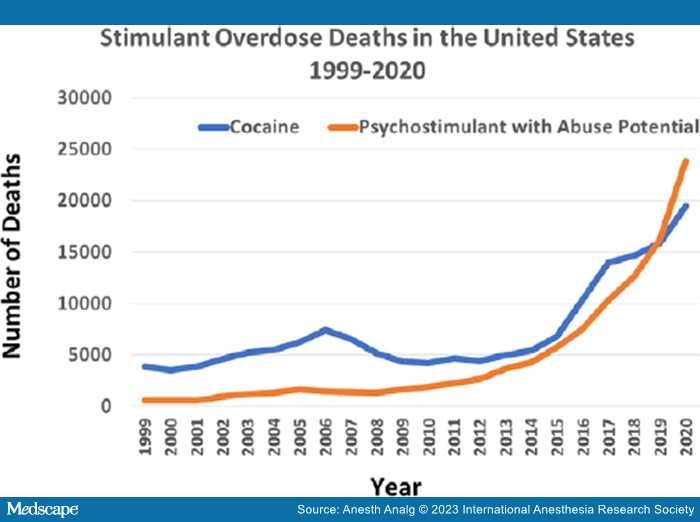
The use of psychostimulants is widespread, with an estimated lifetime prevalence of 7%,[1,2] and psychostimulant-related mortality continues to rise (Figure 1).[3] The well-known stimulants methamphetamine and cocaine remain readily accessible as new substances are synthesized. Escalating legal use of prescription psychostimulants, particularly treatment of attention deficit hyperactivity disorder (ADHD) and even narcolepsy, has contributed to increased nonmedical use.[4] Psychostimulants may play a role in the management of chronic noncancer pain as well, especially pain of neuropathic origin.[5]
Figure 1.
Increase in psychostimulant use. Overdose deaths with cocaine and psychostimulants in the United States from 1999 to 2020. Over the time period, deaths have increased, with a rapid escalation over the past 5 years. From 2019 to 2020, the rate of drug overdose deaths involving cocaine increased 22%, while overdose deaths involving psychostimulants with abuse potential increased 50%. Cocaine is the blue line, and psychostimulants with abuse potential are the orange line. Psychostimulants with abuse potential include such drugs as methamphetamine, amphetamine, and methylphenidate. Deaths may involve more than 1 drug. The percentage of drug overdose deaths that identified the specific drugs involved varied by year, ranging from 75% early to 94% in 2020. Adapted from Hedegaard et al.3
Many psychostimulants used recreationally act by increasing catecholamine levels, generally by increasing release or blocking reuptake, while others are more varied in their neurotransmitter activity. Some compounds display both psychostimulant and hallucinogenic activity through a combination of pharmacological activities.
Considering the ubiquity of psychostimulants, anesthesia providers should be familiar with the clinical features of acute intoxication and chronic use. Patients exposed to these substances present for both elective and emergent surgeries. Appreciation of the perioperative implications is essential to effectively manage patients in the safest manner. Herein, we review the pharmacology of these drugs and the considerations of exposure in patients presenting for anesthetic care, particularly focusing on substances with known perioperative implications.
Anesth Analg. 2023;137(3):474-487. © 2023 International Anesthesia Research Society